A Shorter Distance™
(214) 586-0378
A Shorter Distance™
Purpose of this information.
The purpose of this information is to explain the mechanism and cures of autoimmune diseases caused by food allergies or food sensitivities. This requires a reliable blood test to elucidate the food sensitivities followed by a careful reading of the test results. Then healing can begin rather quickly in many cases.
Can food allergies cause autoimmune disease?
Today most doctors are skeptical of food allergies as being the cause of autoimmune diseases. This is understandable because we are not taught about this concept in medical school.
We learned that autoimmune diseases resulted when antibodies, or some part of the immune system, launched an attack on certain tissues in the body, but we never knew why.
We were taught how to help patients with symptoms of autoimmune diseases using drugs, but not how to cure them. We were taught that autoimmune diseases were incurable. So we prescribed steroids and anti-cancer drugs to suppress the immune system response. These drugs helped in many cases, for varying periods of time, but had serious side effects. Thirty years later, the same drugs are still being used!
Doctors acknowledge a similar concept found in the disease called the rheumatic fever.
The concept of antibodies to one allergen cross-reacting with a particular body tissue is not unknown to doctors. Every doctor is familiar with rheumatic fever as being an occasional cause of heart, skin, joint and brain damage based on an autoimmune response. They understand that a person with strep throat or scarlet fever can develop antibodies against a protein of the causative bacteria (group A Streptococcus). These antibodies can sometimes attack both the bacteria as well as heart, skin, joints, and brain tissue. In order to help prevent a reoccurrence of the strep infection, it is common for doctors to place the patient on antibiotics for many years, or even decades. The doctors do not want the patient to become infected again with the Streptococcus bacteria because they know this could result in more damage from additional exposure to the offending allergen.
So, yes, doctors are fully aware of a possible cross-reaction of antibodies to one allergen that can attack what appears, to the untrained eye, to be a different tissue. In reality the antibody is not messed up, it is doing exactly as it was programmed to do. It recognizes a particular amino acid sequence in the bacteria that is identical to the amino acid sequence in either joint, skin, brain or heart tissue. So it attacks both. It performs its job perfectly.
Nevertheless, my colleagues and I are still taught to control symptoms, with drugs, rather than to achieve ultimate healing of the patient. There are many reasons for this.
Doctors have been disheartened by incompetent laboratories.
The few doctors that were open to the food allergy concept as being the cause of autoimmune diseases have been blind-sided by unreliable laboratories providing test results that did not help their patients. It makes no difference how conscientious the patient may be in avoiding incorrectly identified allergic foods by incompetent laboratories. A few failures like this and my colleagues steer clear of this concept. They simply give up on it.
Treating the symptoms versus the cause.
Imagine a woman who goes to the doctor complaining of hand pain. She has been continuously hitting her hand with a hammer. The doctor suggests pain medicine, which helps. Each time she goes to the doctor the hand looks worse, but the pain is getting a little better, for a while anyway. Eventually both doctor and patient agree the only solution is to amputate the hand before the patient dies of gangrene. Neither one seems to think of the idea of getting rid of the hammer. It seems so odd, but this is exactly what is happening with symptom-control medicine in the treatment of all autoimmune diseases.
Consider the diagnosis of Meniere’s disease.
This disease involves the inner ear and can cause pain in the ear, severe cases of dizziness or loss of balance, hearing loss, nausea and vomiting. The hearing loss and ringing in the ears can become constant over time.
The current mainstream belief is that the cause of Meniere’s disease is stress, overwork, fatigue, emotional distress, additional illnesses, pressure changes, certain foods, and too much salt in the diet.
Even the famous medical institutions offer the following information on their websites: No cure exists for Meniere's disease. They say that a number of treatments can help reduce the severity and frequency of vertigo episodes, but there are not any treatments for the hearing loss. Medications injected into the middle ear, and then absorbed into the inner ear, may improve vertigo symptoms.
They say that if vertigo attacks associated with Meniere's disease are severe and debilitating, and other treatments do not help, then surgery might be an option such as the endolymphatic sac surgical procedure. The endolymphatic sac plays a role in regulating inner ear fluid levels. During the procedure, the endolymphatic sac is decompressed, which can alleviate excess fluid levels. In some cases, this procedure is coupled with the placement of a shunt, a tube that drains excess fluid from your inner ear.
Another surgical procedure offered is the labyrinthectomy surgical procedure. With this procedure, the surgeon removes the balance portion of the inner ear, thereby removing both balance and hearing function from the affected ear. This procedure is performed only if you already have near-total or total hearing loss in your affected ear.
And a third surgical procedure suggested is the vestibular nerve section surgical procedure. This procedure involves cutting the nerve that connects balance and movement sensors in your inner ear to the brain (vestibular nerve). This procedure usually corrects problems with vertigo while attempting to preserve hearing in the affected ear.
An exciting case history of a patient with Meniere’s Disease.
Now consider the actual case of a 29 year-old man with Meniere’s disease. This man had been having attacks occasionally for over 4 years, but the attacks were occurring daily for the past 4 months, and he was unable to function, feeling hopeless and suffering greatly. He had spent thousands on diagnostic tests and was told he had an incurable disease. His doctor's recommendation was to avoid salt, but he had no improvement avoiding salt.
And a third surgical procedure suggested is the vestibular nerve section surgical procedure. This procedure involves cutting the nerve that connects balance and movement sensors in your inner ear to the brain (vestibular nerve). This procedure usually corrects problems with vertigo while attempting to preserve hearing in the affected ear.
He got rid of the hammer. So simple.
How are foods similar to my nerves or my gut proteins?
Many ask why do egg allergies, for example, cause Ulcerative Colitis in one patient, but cause Multiple Sclerosis in another? The reason may be that there are many different types of proteins in eggs. And antibodies (allergy) may develop to one of the proteins, or actually a portion of one of the partially-digested proteins, that have an identical amino acid sequence found in the colon tissue or the myelin sheath of the nerves. The first would cause Ulcerative Colitis where as the second would cause Multiple Sclerosis.
What is the root cause of the allergies?
Now, you may be asking, what causes the food allergies in the first place and why are autoimmune diseases increasing by 10-15% per year? The answer is simple: leaky gut caused by genetically modified wheat with high gluten content. Leaky gut is most common in the USA and UK. It is less common in Europe. The reason is because the genetically modified wheat, via extensive cross-hybridization, is primarily available in the USA and UK.
I am convinced that most chronic conditions are the result of leaky gut-induced food allergies involving the IgA and IgG antibodies, the delayed arm of the immune system.
Is reintroducing a food allergen into your diet a logical consideration?
Some of my colleagues believe that after an allergic food has been avoided for an extended period of time it may be reintroduced into the diet without harm. They believe this because no adverse effect is observed sometimes. However, if another study is done to check food antibodies, the patient still has the antibodies to that food.
Here’s the issue. When the study is done initially, multiple food allergens may be detected. For instance, a patient may be allergic to diary and eggs, and present with arthritis signs and symptoms. It may be only the eggs that are causing the arthritis. So if diary is reintroduced, obviously no adverse effects will be observed in respect to the arthritis.
Meanwhile, the dairy may be causing silent damage, for instance damage to the kidneys, that may not be noticed for decades when the patient eventually develops essential hypertension. Early on the kidney damage might be seen by a microscopic examination of the urine, but usually it goes undetected.
Do not reintroduce known allergic foods. Avoid all allergic foods even if they are causing no apparent signs or symptoms.
Your immune system has the memory of an elephant.
When you get most virus infections, you will never get that same disease again because your immune system on constant alert and has the ability to expand its response rapidly upon the appearance of a previously encountered virus. It does the same thing with food allergens. Do not underestimate your immune system; it is ever vigilant
Are some foods more likely to cause allergies?
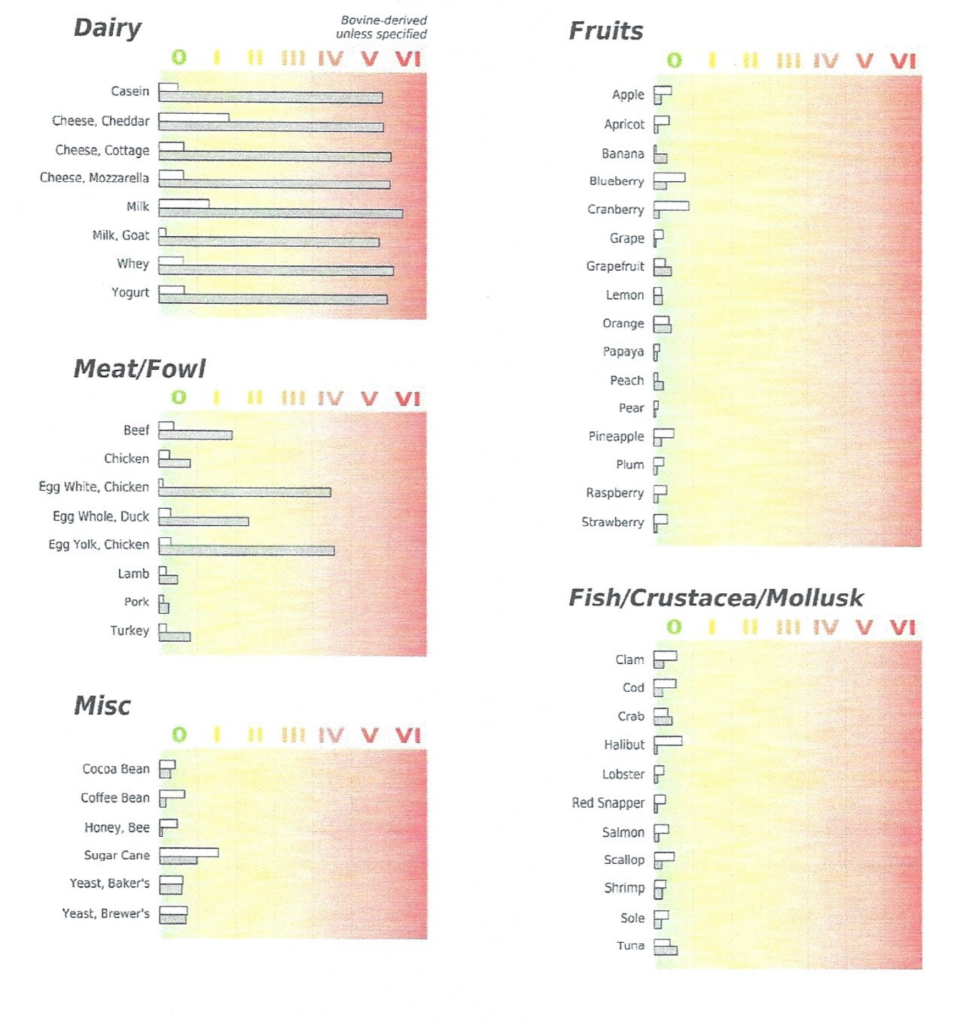
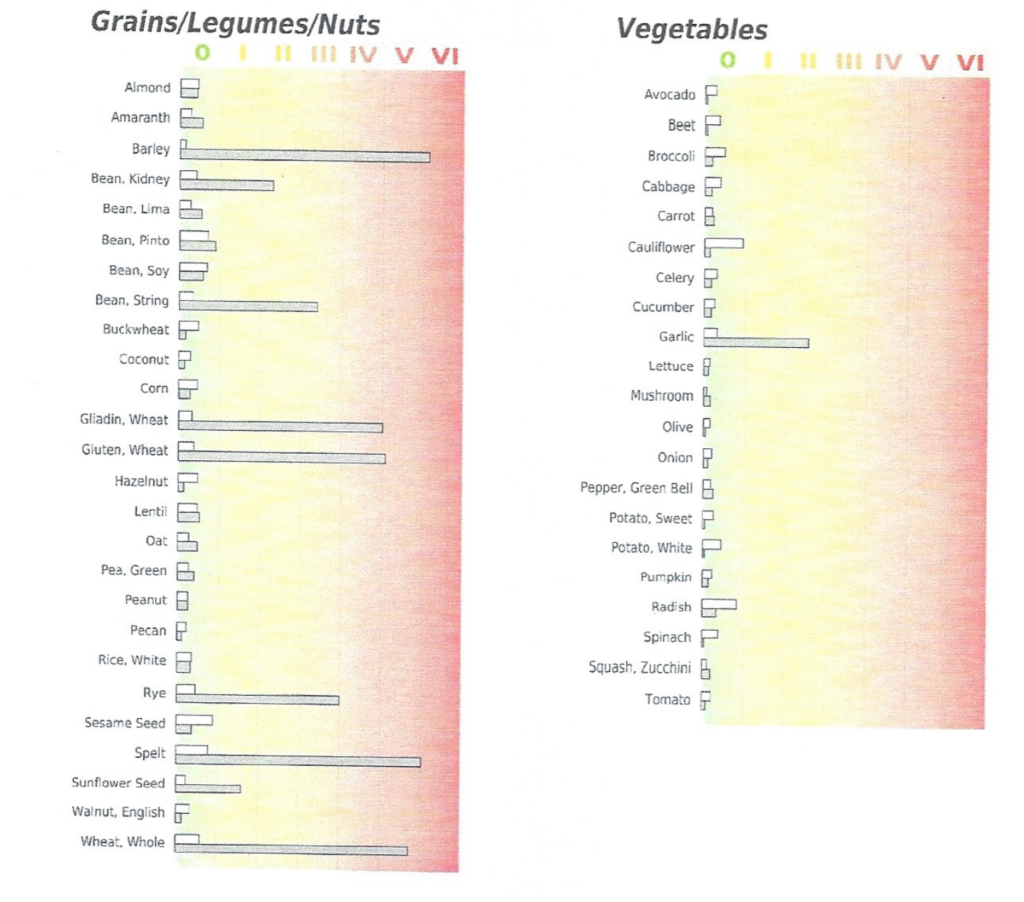
Based on probabilities and past experience, and a good laboratory test, we can have a general idea which food is causing the problem or problems observed, since some foods are the more probable culprits than others; fruits and vegetables tend to be less of a problem, even when showing up as an allergy, due to the lower protein content in them. A person can only develop an allergy to a protein molecule.
Is a 95% success rate in avoiding your food allergen adequate for improvement in your condition?
Not really. Imagine you are walking through a forest laden with land mines. How would your body feel if you only stepped on 5% of them? 100% is required to survive! Less than that will cause damage to some part of your body. Do not step on a single land mine
Choice of a laboratory and a food sensitivity test.
I use the USBioTek Laboratory. USBiotek’s least expensive food sensitivity blood test is $159, for 96 food groups, for IgG antibodies. USBiotek’s most expensive test is $429, for 208 food groups, for both IgG and IgA antibodies. The main advantage of the more expensive test is that it may provide more non-reactive food choices that you may consume, and it may detect more foods to which you are sensitive. But even the least costly test is quite valuable. USBioTek can send you either the finger prick test that you can do at home, or the serum test that requires your blood being drawn at your local hospital or lab. These prices are the wholesale doctor prices paid by the patient directly to USBioTek for which the doctor receives no compensation. Some insurance plans may cover the cost of the test. USBioTek ships their test kits in the USA and Canada. After you return the kit to USBioTek, it takes about 10 days to get the results emailed to you.
Evaluation of food sensitivity testing.
At first glance, it may appear straightforward to evaluate food sensitivity test results. Just avoid the offending foods, right? Not exactly.
The safest course of action is to choose the foods that (1) were tested, (2) were eaten in the last month, and (3) showed low sensitivity. The reason for this course of action is as follows. If you tested negative for a food that you have not eaten recently, you might be sensitive to it but the test is not showing it as reactive because you have not had recent exposure to it. Over time, weeks to months, the antibody levels will decrease to sensitive foods if those foods are avoided. So if you are sensitive to dairy, but have not eaten dairy for several months, your test may not show any reactivity to dairy.
Keep in mind that IgG antibodies have a half-life of 25 days; IgA antibodies have a half-life of 5 days. This means that only very recent exposure will show IgA reactivity, whereas less recent exposure will show IgG reactivity.
In addition, even if gluten foods are not shown as reactive, they should be avoided to prevent gut damage which can result in developing sensitivity to even more food groups.
What if a good food sensitivity test is not available in your country or is too expensive?
If you cannot get a good test, the best option is to avoid the most common allergic foods which are dairy (cow milk, cheese, butter, etc), eggs, gluten (wheat, oats, barley and rye), cane sugar, and yeast. If you have easily observable signs and symptoms such as a skin rash or arthritis, these conditions will normally worsen within 72 hours of eating an offending food and lessen within 4 days of avoiding the offending food.
Common pitfalls when dealing with food sensitivities.
The most common pitfalls are supplements which may contain fillers to which you are sensitive. Sometimes the capsule of the supplement can be the culprit. Medicines can also contain allergic fillers. Spices, and sauces are also known to be allergens and must be avoided unless shown to be non-reactive by the testing. More detais can be found at the Hidden Food Ingredients
Additional valuable information and protocols.
Additional valuable information is available to help you deal with food sensitivities and autoimmune issues. You may request this additional information on this form and it will be sent to you by email: Additional Information
What constitutes an autoimmune diagnosis?
A patient’s autoimmune diagnosis is based various immune-related tests, and on which signs and symptoms occur in the organs being damaged by antibodies resulting from the particular food allergy. Here are some examples: Autoimmune Conditions
Medical literature supports food allergy causation for autoimmune diseases.
The following are just a few of the published studies in medical journals that support the idea of food allergies as a causative mechanism in autoimmune conditions.
Delayed Immunomodulatory Effect of Cow Milk-Free Diet in Ménière’s Disease. J Am Coll Nutr. 2018 Feb;37(2):149-153. https://www.ncbi.nlm.nih.gov/pubmed/29087236
Allergic and Immunologic Features of Ménière’s Disease. Otolaryngol Clin North Am. 2011 Jun;44(3):655-66. https://www.ncbi.nlm.nih.gov/pubmed/21621052
A vegan diet free of gluten improves the signs and symptoms of rheumatoid arthritis: the effects on arthritis correlate with a reduction in antibodies to food antigens. Rheumatology (Oxford) 2001 Oct;40(10):1175-9. https://pubmed.ncbi.nlm.nih.gov/11600749/
Association between food allergy and ankylosing spondylitis: An observational study. Medicine (Baltimore). 2019 Feb;98(6). https://pubmed.ncbi.nlm.nih.gov/30732197/
Food-specific IgGs Are Highly Increased in the Sera of Patients with Inflammatory Bowel Disease and Are Clinically Relevant to the Pathogenesis. Internal Med. 2018 Oct 1;57(19):2787-2798. https://pubmed.ncbi.nlm.nih.gov/29780153/
Slipping through the Cracks: Linking Low Immune Function and Intestinal Bacterial Imbalance to the Etiology of Rheumatoid Arthritis. Ann Saudi Med. Nov-Dec 2016;36(6):386-390. https://pubmed.ncbi.nlm.nih.gov/25861466/
Prevalence of IgG-mediated food intolerance among patients with allergic symptoms. Autoimmune Dis. 2015;2015:636207. https://pubmed.ncbi.nlm.nih.gov/27920409/
Food Intolerance Prevalence in Active Ulcerative Colitis in Southwest China. Asia Pac J Clin Nutr. 2016;25(3):529-33. https://www.ncbi.nlm.nih.gov/pubmed/27440687
Food Exclusion Based on IgG Antibodies Alleviates Symptoms in Ulcerative Colitis: A Prospective Study. Inflamm Bowel Dis. 2018 May 16. https://www.ncbi.nlm.nih.gov/pubmed/29788288
A Shorter Distance ™
(214) 586-0378
Copyright (c) 2021 A Shorter Distance ™